ACA Section 1557 Violations: Potential Consequences for Health Plans
Understand ACA section 1557 and its importance for health plans
Section 1557 of the Affordable Care Act (ACA) represent a significant civil rights provision that now impact health plans across the United States. This non-discrimination rule prohibit discrimination on the basis of race, color, national origin, sex, age, or disability in health programs or activities that receive federal financial assistance. For health plans, compliance with section 1557 is not optional — it’s a legal requirement with serious consequences for violations.
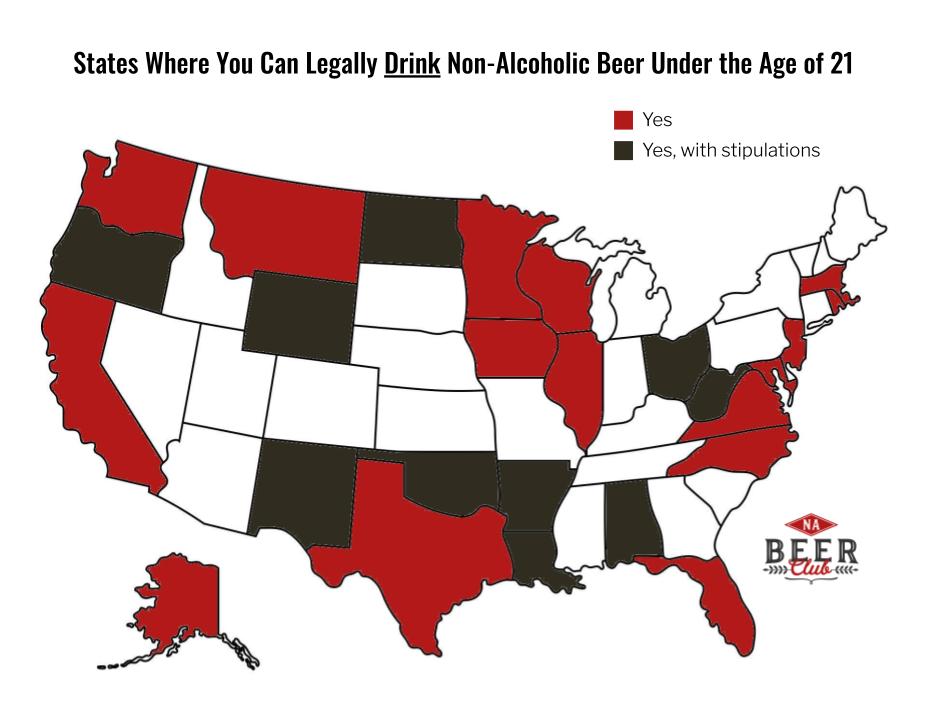
The scope of section 1557 extend to most health insurers, third party administrators, and employer sponsor health plans that receive federal funds. This includes plans participate in the health insurance marketplace, medicare advantage plans, medicaid manage care organizations, and many others that receive federal financial assistance.
Financial penalties for section 1557 violations
When health plans violate section 1557, they face substantial financial consequences. These penalties are design to ensure compliance and can importantly impact a health plan’s bottom line.
Civil monetary penalties
The office for civil rights (oOCR)within the department of health and human services ( (sHHS)ve the authority to impose civil monetary penalties for section 1557 violations. These penalties can vary base on factors such as:
- The nature and extent of the violation
- The harm result from the violation
- The size of the health plan
- The history of prior compliance issues
- The financial condition of the cover entity
Monetary penalties can reach into the millions of dollars for serious or repeat violations. The OCR consider each instance of discrimination as a separate violation, potentially multiply the financial impact for systemic issues.
Settlement agreements and corrective action plans
Beyond direct penalties, health plans find in violation of section 1557 much face settlement agreements that include significant financial components. These settlements oftentimes require:
- Payment of damages to affected individuals
- Funding for monitoring and compliance programs
- Investments in staff training and policy development
- Costs associate with external auditors or compliance monitors
The financial burden of these settlement agreements oftentimes exceed the initial penalties and can strain operational budgets for years follow a violation.
Legal consequences and litigation risks
Section 1557 create significant legal exposure for health plans beyond regulatory penalties. Understand these legal consequences is crucial for risk management.
Private right of action
Section 1557 provide individuals with a private right of action, mean those who believe they’ve been discriminated against can file lawsuits direct against health plans. Thiscreatese substantial litigation risk, as these cases can result in:
- Compensatory damages for affected individuals
- Payment of plaintiffs’ attorney fees
- Punitive damages in cases of intentional discrimination
- Class action lawsuits represent numerous affected individuals
The financial impact of private litigation can far exceed regulatory penalties, especially in class action scenarios where damages are multiply across many affected individuals.
Injunctive relief and court order remedies
Courts hear section 1557 cases have broad authority to order remedies beyond monetary damages. Health plans find in violation may be subject to:
- Court order changes to policies and procedures
- Mandatory training programs
- External monitoring and reporting requirements
- Specific performance requirements to remedy discriminatory practices
These court order remedies oftentimes require significant operational changes and ongoing compliance costs that affect the health plan’s ability to operate expeditiously.

Source: brailleworks.com
Operational and administrative consequences
Beyond direct financial penalties and legal consequences, section 1557 violations trigger operational impacts that can essentially alter how a health plan functions.
Corrective action plans
The OCR typically require health plans with section 1557 violations to implement detailed corrective action plans (caps ) These plans impose significant operational burdens include:
- Comprehensive policy revisions and updates
- Development of new compliance programs
- Implementation of regular staff training
- Creation of new grievance procedures
- Regular reporting to regulatory authorities
- Periodic audits and assessments
The administrative costs of implement and maintain these corrective action plans represent a substantial ongoing expense that impact operational efficiency and diverts resources from other priorities.
Enhance oversight and monitoring
Health plan with section 1557 violations face increase regulatory scrutiny that extend beyond the specific violation. This enhanced oversight typically includes:
- More frequent regulatory audits
- Detailed compliance reporting requirements
- Mandatory external monitoring
- Heighten scrutiny of other operations and practices
This increase regulatory attention create additional administrative burden and compliance costs that can persist for years after the initial violation.
Reputational damage and market consequences
The impact of section 1557 violations extend beyond direct penalties to affect a health plan’s market position and relationships with stakeholders.
Public disclosure and media coverage
The OCR publically announce enforcement actions and settlements relate to section 1557 violations. This public disclosure oftentimes result in:
- Negative media coverage at local and national levels
- Public perception of discriminatory practices
- Social media amplification of the violation
- Last online records of non-compliance
The reputational damage from these public disclosures can importantly impact member enrollment, provider relationships, and employer contracts.
Loss of market share and business opportunities
Health plan with section 1557 violations much experience tangible business consequences include:
- Reduced enrollment during open enrollment periods
- Difficulty secure or maintain government contracts
- Challenges in employer group sales
- Increase scrutiny from potential business partners
- Higher costs for business relationships due to perceive compliance risks
These market consequences can persist longsighted after the violation has been remediated and may represent the about significant long term impact ofnon-compliancee.
Federal funding and program participation risks
For health plans receive federal financial assistance, section 1557 violations create existential risks relate to program participation and funding.
Loss of federal financial assistance
The virtually severe consequence for persistent or egregious section 1557 violations is the potential termination of federal financial assistance. This can include:
- Termination of medicare or medicaid contracts
- Removal from health insurance marketplace participation
- Loss of other federal funding or subsidies
- Exclusion from federal employee benefit programs
For many health plans, specially those with significant government program participation, the loss of federal financial assistance could represent an existential threat to business viability.
Program exclusion and debarment
In the nearly serious cases, health plans and their executives may face:
- Temporary or permanent exclusion from federal healthcare programs
- Debarment from government contracting
- Limitations on future program participation
- Enhance scrutiny for re-entry into federal programs
These program participation consequences extend beyond the immediate financial impact to affect long term business strategy and viability.
Specific violation categories and their consequences
Different types of section 1557 violations may trigger specific consequences base on the nature of the discrimination.
Language access violation
Failure to provide appropriate language assistance services to individuals with limited English proficiency can result in:
- Mandate implementation of comprehensive language access programs
- Requirements to provide translate materials in multiple languages
- Obligation to contract with interpreter services
- Monitoring of communication effectiveness
These remedies oftentimes require significant ongoing operational expenses and system changes.
Disability accommodation violation
Discrimination against individuals with disabilities can lead to:
- Requirements for facility modifications and accessibility improvements
- Mandated provision of auxiliary aids and services
- Development of disability accommodation policies and procedures
- Staff training on disability rights and accommodations
The costs of physical modifications and accommodation programs can be substantial and may require capital investments beyond normal operational budgets.
Sex discrimination violation
Violations relate to sex discrimination, include gender identity and sexual orientation, may result in:
- Required coverage of antecedent exclude services
- Revision of benefit designs and coverage policies
- Implementation of non-discrimination training programs
- Development of specific protocols for gender affirm care
These remedies oftentimes require fundamental changes to benefit design and coverage policies that affect actuarial calculations and premium structures.
Individual liability for health plan executives
Beyond organizational consequences, section 1557 violations can create personal liability for health plan executives and board members.
Personal liability in enforcement actions
In cases of know or deliberate violations, individual executives may face:
- Personal financial penalties
- Individual naming in lawsuits and enforcement actions
- Potential exclusion from participation in federal healthcare programs
- Professional licensure consequences
This personal liability create significant incentives for executives to ensure organizational compliance with section 1557 requirements.

Source: chlpi.org
Fiduciary duty implications
Health plan board members and executives have fiduciary duties that may be implicated by section 1557 violations:
- Shareholder derivative actions for failure to ensure compliance
- Breach of fiduciary duty claims
- Corporate governance consequences
- Insurance coverage limitations for intentional violations
These fiduciary implications extend the consequences of non-compliance beyond regulatory penalties to affect corporate governance and executive liability.
Proactive compliance strategies to avoid violations
Give the severe consequences of section 1557 violations, health plans should implement comprehensive compliance strategies.
Comprehensive risk assessment
Effective compliance begin with understand potential vulnerabilities:
- Regular audits of policies, procedures, and benefit designs
- Review of member communications and accessibility
- Assessment of provider network adequacy and accessibility
- Evaluation of complaint data and grievance patterns
These risk assessments should be conducted sporadically and whenever significant operational or benefit changes occur.
Policy development and implementation
Health plans should establish clear non-discrimination policies that:
- Explicitly prohibit discrimination on all protect bases
- Establish clear procedures for handle accommodation requests
- Create effective grievance procedures for discrimination complaints
- Define responsibilities for compliance oversight
These policies should be regularly updated to reflect changes in regulatory guidance and enforcement priorities.
Staff training and awareness
Ensure that all staff understand section 1557 requirements is essential:
- Regular training on non-discrimination requirements
- Specialized training for customer face staff
- Leadership education on compliance responsibilities
- Ongoing update on regulatory changes and enforcement trends
This training should be documented and refresh regularly to maintain awareness and demonstrate compliance commitment.
Conclusion: the imperative of section 1557 compliance
The consequences of section 1557 violations for health plans are far reach and potentially devastating. From direct financial penalties to operational disruptions, reputational damage, and yet existential threats to business continuity, non-compliance create risks that no health plan can afford to ignore.
The near effective approach is to prioritize compliance through comprehensive policies, regular training, ongoing monitoring, and a culture that value non-discrimination as both a legal requirement and an organizational value. By understand the severe consequences of violations and implement proactive compliance strategies, health plans can avoid the substantial risks associate with section 1557 non-compliance while substantially serve their diverse member populations.
MORE FROM searchcritic.com